“Brain fog” is an informal term for feeling mentally sluggish or “cloudy.” It is a collection of symptoms that include: trouble focusing or tracking tasks, forgetting words or having a tough time remembering the right word for a situation, short-term memory slips (e.g. walking outside with your thermos and keys in your hand only to realize you are holding your coffee mug from breakfast and you left your keys and thermos on the counter), slowed thinking, feeling “spaced out,” and struggling with decision fatigue. [1, 3].
Brain fog is common, frustrating—and usually fixable. Start with better sleep hygiene, stress-coping skills, daily movement, hydration, and a balanced, fiber-rich diet to support the gut–brain axis.
Read on to learn about what causes brain fog, signs you might be struggling with it, and how to heal the gut-brain connection to improve your cognitive health.
What Causes Brain Fog?
Sleep Debt, Stress & Mental Load
Brain fog can be caused by not getting enough sleep, not having a consistent sleep schedule, insomnia, chronic stress, and constantly needing to multitask. If your executive function (the brain’s attention and decision-making systems) is overloaded from a lack of sleep, it will impair your working memory, causing you to feel even more stressed out, and contribute to feelings of mental ‘cloudiness’ [10, 11].
Nutrition, Blood Sugar Swings & Hydration
Low blood sugar is another cause of brain fog. Long gaps between meals, low protein/fiber intake, ultra-processed foods, excessive sugar consumption, dehydration, and alcohol can all contribute to energy dips, leading to a foggy outlook.
One way to stabilize blood sugar and clear brain fog is to eat balanced meals and stay adequately hydrated to start. Nutrition may be the key to fixing your brain fog if you haven’t added a new medication to your daily routine or been diagnosed with a disease associated with brain fog [6].
Medications and Hormones
Common culprits include sedating antihistamines, pain medications, or certain mental health medicines such as mood stabilizers or antipsychotics. Changes or increases in dosing can also blur thinking.
Hormone shifts (PMS/PMDD, pregnancy/postpartum, perimenopause/menopause, low testosterone) can trigger or worsen fog for some people. If brain fog begins after starting a new medication or around hormonal transitions, discuss it with your clinician [1].
Infection, Inflammation & Post-Illness Recovery
After a viral or bacterial illness—famously after COVID-19—many people experience lingering fatigue and cognitive slowdown (including processing speed and attention) as inflammation subsides and sleep returns to normal. COVID-19-related brain fog can last weeks or months (“long-COVID”) [12].
Underlying Conditions to Rule Out
Thyroid disorders, iron or B12 deficiency, anemia, sleep apnea, depression/anxiety, ADHD, diabetes or glucose dysregulation, autoimmune disease flares, chronic pain, and substance use can all present with “fog.” Persistent or worsening brain fog warrants a clinical workup to check these drivers [1].
The Gut–Brain Connection: Why Your Microbiome Affects Clarity
Your gut and brain communicate bidirectionally via nerves (vagus), hormones, immune messengers, and microbial metabolites. Gut microbes help produce brain-active compounds and SCFAs that influence microglia—brain immune cells involved in attention, mood, and cognition [5, 7].
Patterns rich in vegetables, legumes, fruits, whole grains, nuts, olive oil, fish, and fermented foods (Mediterranean-style) tend to support microbial diversity and steadier energy [6].
Fatigue and Mental Fog: Why Tiredness Blurs Thinking
Sleep Quality vs. Sleep Quantity
Seven to nine hours is a good target, but sleep depth and regularity matter. Irregular schedules fragment sleep and erode attention the next day. Improving sleep quality consistently improves cognitive performance and reduces daytime “fog” [10].
Energy Availability, Iron/B12 & Thyroid Considerations
Low iron (with or without anemia), low B12, and thyroid imbalance can feel like “I slept but still feel wiped out.” Your doctor can order simple labs and follow-ups if deficiencies are found.
Pacing, Recovery & Light Activity
If you’re recovering from illness or burnout, pace yourself: break big tasks down into manageable chunks, take small breaks, and stand up and walk around when you can. Mind-body techniques paired with graded activity can help calm the stress response that fuels fog.
How to Get Rid of Brain Fog (Evidence-Based)
Brain fog can be addressed with several lifestyle changes, nutritional approaches, stress management tools, and professional treatment. If you develop acute symptoms—sudden severe confusion, slurred speech, facial droop, incoherence, high fever, new weakness/numbness, severe headache, or suicidal thoughts—seek emergency care immediately.
Some of the ways to reduce brain fog include:
- Set your alarm, don’t sleep through it: See sunlight within an hour of waking to reinforce circadian rhythms.
- Choose to move: Brisk walking 20 to 30 minutes or “movement snacks” (5–10 minutes) during the day.
- Add brief relaxation reps: Physiological sighs or box breathing between tasks.
- Pre-bed wind-down: Dim lights, no work, limit screens.
- Aim for 20g to 40 g of Protein per meal, make half your plate plants, reduce processed carbs, or pair carbs with protein/fat [6].
- Time-block deep work in 25–50 minute chunks: put your phone away, check 2–3 times daily.
- Cap caffeine at 200–300 mg/day and avoid it by early afternoon. Even small amounts of alcohol can fragment sleep and impair next-day clarity.
- Seek help if brain fog lasts >2 weeks—especially with loud snoring/paused breathing (possible sleep apnea), mood or attention changes, or slow recovery after infection.
Clinicians can screen for anemia, B12 deficiency, thyroid function issues, glucose disorders, sleep disorders, medication side effects, and post-infection complications [1, 12].
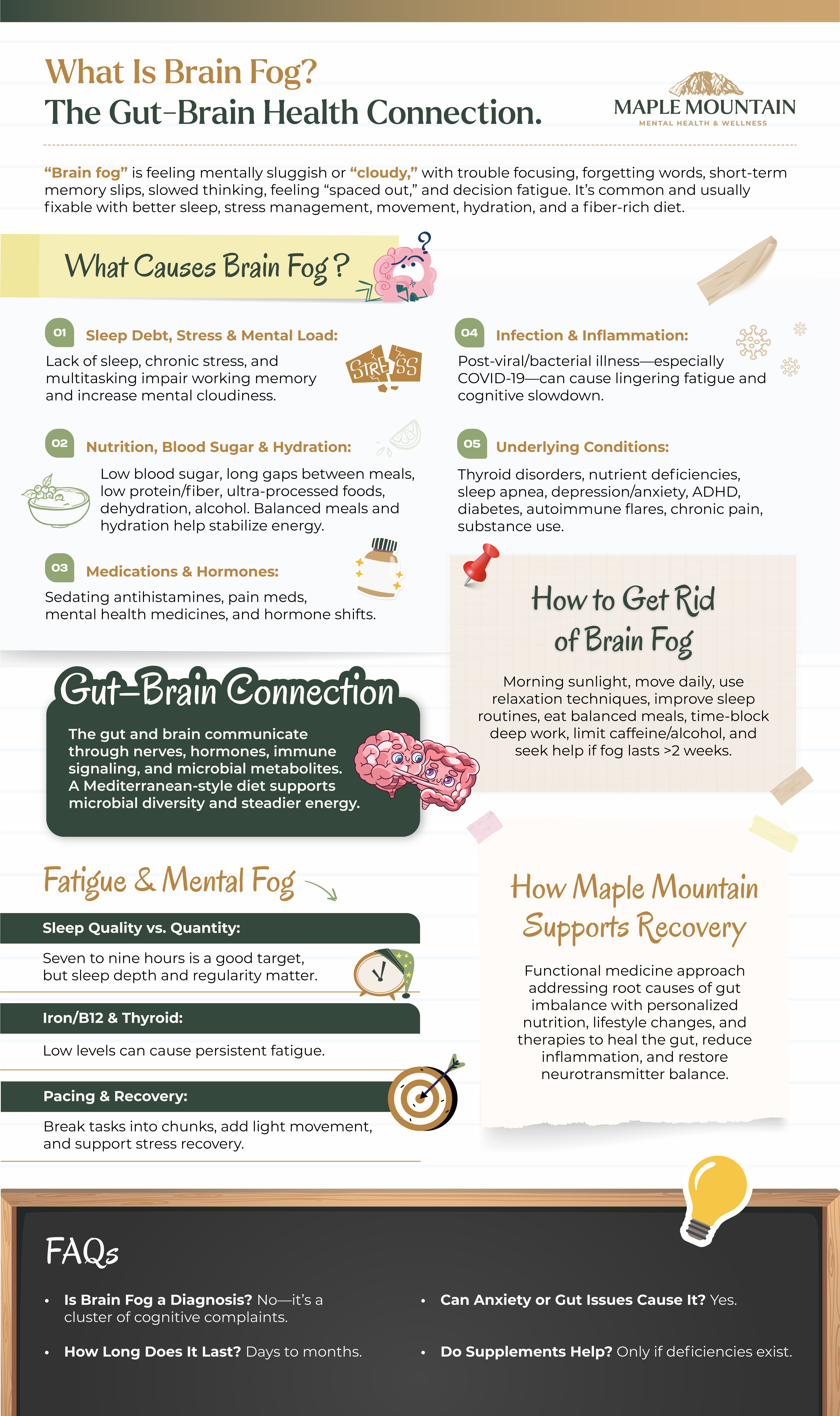
How Maple Mountain Supports Gut Health Restoration and Recovery with Functional Medicine
Maple Mountain Mental Health & Wellness supports gut health restoration and recovery through a functional medicine approach that addresses the root causes of gut imbalance. Our team creates personalized treatment plans incorporating targeted nutrition, lifestyle modifications, and advanced therapies to heal the gut lining, reduce inflammation, and restore neurotransmitter balance.
Our focus on individualized care empowers clients to rebuild gut health while supporting overall physical and mental well-being, helping patients achieve sustainable healing and improved quality of life.
Contact our admissions team today to connect with an alcohol treatment program.
FAQs
Is Brain Fog a Diagnosis?
No. It’s a term for a cluster of subjective cognitive complaints; treatment targets the underlying contributors (sleep issues, mental health, medical causes, nutrition, medication effects, infections) [1, 3].
How Long Does Brain Fog Last?
It can follow a bad night’s sleep or a severe infection and last for weeks. In long-COVID and some chronic conditions, recovery is gradual and can last for months [12].
Can Anxiety or Gut Issues Cause Brain Fog?
Yes. Anxiety consumes attention and working memory; GI inflammation and dysbiosis can amplify fatigue and “cloudy” thinking via immune, neural, and hormonal pathways [1].
Do Supplements Help with Brain Fog?
They can if there’s a deficiency (iron, B12, vitamin D). Omega-3s and magnesium have modest support in some contexts, but many “nootropics” are over-hyped. Prioritize sleep, nutrition, movement, and mental-health care; integrative programs often assess nutrition, hormones, and GI health when appropriate [6].

Sources
- Cleveland Clinic. (2024, May 14). Brain fog: What it is, causes, symptoms & treatment. https://my.clevelandclinic.org/health/symptoms/brain-fog
- Detroit Medical Center. Brain fog and when to worry. https://www.dmc.org/healthy-living/corporate-content/when-should-you-worry-about-brain-fog
- Wikipedia contributors. (2025). Clouding of consciousness. https://en.wikipedia.org/wiki/Clouding_of_consciousness
- Denno, P., Zhao, S., Husain, M., & Hampshire, A. (2025). Defining brain fog across medical conditions. Trends in Neurosciences, 48(5), 330–348. https://doi.org/10.1016/j.tins.2025.01.003
- Johns Hopkins Medicine. The brain–gut connection. https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-brain-gut-connection
- Harvard Health Publishing. (2023, July 18). The gut-brain connection. https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection
- Cleveland Clinic. What is the gut–brain connection? https://my.clevelandclinic.org/health/body/the-gut-brain-connection
- Colombo, A. V., et al. (2021). Microbiota-derived short chain fatty acids modulate microglia and promote Aβ plaque deposition. eLife, 10, e59826. https://doi.org/10.7554/eLife.59826
- Caetano-Silva, M. E., et al. (2023). Inhibition of inflammatory microglia by dietary fiber and short-chain fatty acids. https://pmc.ncbi.nlm.nih.gov/articles/PMC9935636/
- Alhola, P., & Polo-Kantola, P. (2007). Sleep deprivation: Impact on cognitive performance. https://pmc.ncbi.nlm.nih.gov/articles/PMC2656292/
- Khan, M. A., Zahir, F., & Shafique, A. (2023). The consequences of sleep deprivation on cognitive performance. https://pmc.ncbi.nlm.nih.gov/articles/PMC10155483/
- News-Medical. (2025, Feb 28). The science behind long COVID brain fog. https://www.news-medical.net/health/The-Science-Behind-Long-COVID-Brain-Fog.aspx
